If you're new here, you may want to subscribe to my RSS feed. Thanks for visiting!
According to Food Safety.gov, two of the most common foodborne illnesses are Listeria and E.coli. Dagny Taggart has already written an especially informative article on listeria and a listeria outbreak in the spring of this year that I would caution everyone to read carefully. This dangerous bacterium is fatal in up to 30% of cases and a listeria infection is not easily preventable.
E.coli, however, baffles my mind.
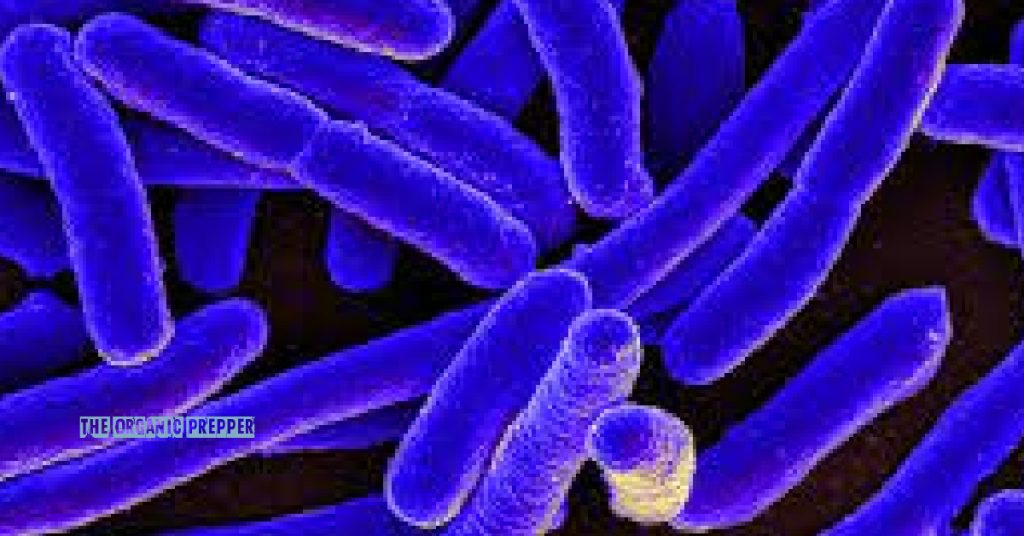
E. coli bacteria can be found just about everywhere.
Escherichia coli bacteria was first discovered in 1885 in the human colon by a German doctor named Theodor Escherich using infant fecal samples. It was initially called Bacterium coli, but the name was later changed to honor its discoverer. Most of us are very aware of Escherichia coli, or E. coli for short, and while it’s true that most are harmless, there are several that aren’t, and they’ve been the content of many news reports and have caused many scares. From fruits and vegetables to meats, these bacteria have run the gamut and don’t seem to be losing steam anytime soon. E. coli are bacteria that are found in the intestines of animals, the environment, and in food, and can cause a myriad of infections in the human body.
An article on Medscape written by Tarun Madappa, MD, MPH, states E.coli is one of the most frequent causes of many bacterial infections, including urinary tract infections, gallbladder complications (cholecystitis), pneumonia, septic arthritis, brain abscesses, infection in the bones, cellulitis, sepsis (bacteremia), inflammation of the bile duct system, meningitis in infants, and more.
Some E. coli strains are more dangerous than others.
Shiga Toxin-producing E.coli (STEC) is the one most commonly heard about in the news in regards to foodborne outbreaks. It comes from the guts of animals and usually affects us through cattle – from ingesting contaminated beef, drinking water contaminated by runoff from stockyards, eating vegetables contaminated by runoff, and being in contact with the animal and/or its environment, or other people who are infected via the oral/fecal route.
Enterotoxigenic E. coli is the version most commonly noted as causing “Travelers Diarrhea”, and is transmitted by food or water contaminated with, you guessed it, animal or human feces. To date, however, the most worrisome and worst type of E. coli is Escherichia Coli 0157: H7.
Enterohemorrhagic E. coli O157: H7 induces illness secondary to its production of Shiga toxin that causes a range of gastrointestinal illnesses, from watery diarrhea to hemorrhagic colitis. E. coli 0157: H7 induces enterohemorrhagic disease that can cause systemic illness by hemolytic uremic syndrome, which manifests as hemolytic anemia, thrombocytopenia, and acute renal failure. HUS can result in both acute, potentially life-threatening illness and lifelong, chronic illness. (source)
What does all that technical stuff mean? It means E. coli is dangerous.
Not only are undercooked meat and insufficiently pasteurized dairy products, as well as apple juice, an issue, but so are unwashed fruits and vegetables…as is the forgetful person who cooks up your favorite dinner at your favorite restaurant without washing his/her hands. Unfortunately, the days of swimming or playing in possibly contaminated water like ponds, streams, or lakes, may be gone, as these pose a significant risk as well.
It is important to know how to recognize the symptoms of E. coli infection.
The symptoms of most any E. coli infection are similar to each other and can start as late as two weeks after exposure, and can last two weeks more. Most recover within 10 days. Those symptoms include:
- Diarrhea, sometimes bloody
- Abdominal cramping
- Nausea
- Vomiting
- Mild to moderate dehydration
- Usually no or little initial fever
E. coli 0157: H7, however, includes bloody diarrhea 90% of the time along with more severe dehydration, which can then further increase in severity of symptoms with tachycardia, slow capillary refill, and delirium – particularly in children.
Here’s how E. coli infections are diagnosed and treated.
An important thing to know regarding this type of E. coli is that despite the recommendation by the CDC that all diarrheal samples that are submitted for a culture also undergo screening for E. coli O157:H7, many labs do not routinely screen for this organism, meaning you should insist your doctor request testing for E. coli 0157:H7 if the bacterium is suspected.
The treatment for all cases of E. coli, just like any other type of gastroenteritis, is based on supportive care and maintaining hydration. While medicines like Phenergan/promethazine HCL might possibly help with nausea, neither diarrhea medication (like Imodium) or antibiotics are used, and in fact, might significantly worsen the infection. While doing my research, I did come upon several articles that inferred probiotics would be effective. One such article can be read here.
Alright then, how do we kill E. coli?
On our bodies, again, good old-fashioned soap and water works. On surfaces like kitchen counters, bathrooms, etc., bleach seems to do the trick. Clorox and Lysol wipes both claim to kill E. coli, but I don’t risk it. How about in our food? Does rinsing with water kill it? No. Does freezing kill it? No. But temperatures of 160°F and above do. There are some controversial reports that vinegar, specifically apple cider vinegar, can kill E. coli on fruits and/or veggies but this has yet to be proven.
In a disaster, post-apocalyptic, SHTF world, our best bet is to stay as clean as possible and cook everything we can – including freeze-dried foods – to 160°F. Remember that freezing doesn’t kill E. coli, and it doesn’t require oxygen to live. That means foods dehydrated at a temperature below 160°F, if not cooked well before eating, can pose a risk as well.
Until next time!
What do you think?
Are you concerned about the rise in foodborne illnesses including those caused by E. coli? Are there things you do to avoid contamination in your home? Please share your thoughts in the comments.
About Sandra
Sandra is a published artist, photographer, fellow prepper, and animal advocate.










I’d really like it if you could do PDF files on information such as this so we can download them and keep, but also print a hard copy.
Thank you so much for these articles.
Hi Deborah, you are welcome to highlight my articles then copy and paste them to a word processor like Microsoft Word, then print them for your own use as long as you include The Organic Prepper and my name as the author. 🙂 And thank you for reading them!
more important than ever to know the source of your food and the conditions of its growth and the harvest practices. ie: produce as much of your own as you can and then buy from trusted farmers for the rest.
while washing produce can’t get all the “bad bugs”, it can get some. rinse produce with clean water, spray generously with vinegar and let sit for 5-10 min. rinse again. dry. 3 rinse offs here drain away a lot of germs. vinegar, as an acid, can change the surface pH, which can kill or weaken some germs.
the growth of e coli in ground meat is a direct result of feedlot beef. the 100-150 days of graining beef cattle, in addition to poor conditions for the animal, causes an acidification in the rumens of the cattle. too much acid in that first stomach causes digestive upset–just like acid reflux in humans. cattle don’t get pepsid. what the develop is an altered e coli in their gut–one that can tolerate the acid that used to kill it. that’s also the problem for us. our stomach acid won’t kill it, so we have use scrupulously clean practices and cook beef to above 160 to kill those germs. and think about this: in a beef processing plant, the line moves fast. gut the animal too quickly, you may nick the intestine and spill fecal matter into the abdominal cavity. high pressure hose it out and some of the germs are forced into the meat. if the now-contaminated meat is ground into hamburger and mixed with all the other cows hamburger, now you have thousands of pounds of contaminated beef. that’s how the first e coli outrbeak in a fast food restaurant in washington state occurred. those burgers didn’t quite get to 160 degrees. kidney failures and death resulted.
Thank you!